Vasculitis Types
About Takayasu Arteritis
Last Updated on February 5, 2024
Takayasu arteritis (TAK) is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. TAK affects the body’s largest artery, the aorta, which carries blood from the heart to the rest of the body, and its main branches.
Quick Facts

8 Cases per million worldwide

1 per million US cases

Average age of onset between 15-40

Rare in children

More common in females

More common in women of Asian descent
Takayasu arteritis (TAK) is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. TAK affects the body’s largest artery, the aorta, which carries blood from the heart to the rest of the body, and its main branches.
TAK may or may not cause noticeable symptoms in the early stages of the disease. When early symptoms are present, people may feel generally unwell, with symptoms of mild fever, fatigue, aches and pains, and poor appetite. As the disease progresses, TAK can lead to headaches, chest pain, shortness of breath, high blood pressure, weakness, lightheadedness, and other symptoms.
Early detection and treatment can help lower the risk of serious complications. TAK is usually treated with glucocorticoids such as prednisone and other medications that suppress the immune system, to control inflammation. Even with treatment, TAK is a chronic condition with periods of relapse and remission, so ongoing medical care and monitoring are necessary.
The cause of TAK is not fully understood. Vasculitis is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. Researchers believe an infection may set the inflammatory process in motion, but this is not yet proven. Environmental and some genetic factors may also play a role.
TAK primarily affects Asian women and teenage girls. Nine out of 10 patients are female, with age of onset between 15 and 40 years old. However, the disease can affect children and adults of both sexes, and all races and ethnic groups. Prevalence is estimated at 8.0 per million population.
Symptoms of TAK tend to occur in two stages. In the first stage, patients may feel generally ill, with fatigue, fever, muscle or joint pain, and/or rapid weight loss. However, some may not experience symptoms for months or years—even as inflammation causes damage to blood vessels and organs.
Second-stage symptoms include:
- Pain, numbness or weakness with use of limbs
- Lightheadedness, dizziness, fainting
- Headaches
- Visual disturbances
- High blood pressure (or a discrepancy in blood pressure between arms and/or legs)
- Diminished or absent pulse in the arms and/or legs
- Generalized weakness
- Chest pain
- Shortness of breath/fatigue
Seek medical attention right away if you experience signs of a heart attack (chest or arm pain, shortness of breath, nausea/vomiting) or signs of a stroke (face drooping, arm weakness or difficulty speaking). See your doctor for other symptoms listed above that you may be concerned about.
Even with treatment, damage to vessels may be permanent. Repeated swelling and healing of arteries can lead to complications. Therefore, it is important to follow up with your doctor on a regular basis. Complications can include:
- Hardening and narrowing of the blood vessels
- High blood pressure
- Heart valve disorder (e.g., aortic valve damage)
- Heart failure
- Aortic aneurysm
- Transient ischemic attack (TIA), a “mini stroke” that doesn’t cause permanent damage but serves as a warning sign
- Stroke
- Heart attack
- Pulmonary artery problems
There is no single test for diagnosing TAK, so your doctor will consider several factors including symptoms, a detailed medical history, physical exam findings, laboratory tests, and specialized imaging studies. For most other forms of vasculitis, a biopsy—surgical removal and analysis of suspected tissue—confirms the diagnosis. However, biopsy of large vessels such as the aorta is not feasible unless the patient is undergoing vascular surgery.
- Physical exam: Abnormal exam findings may raise suspicion of TAK: a weak or absent pulse in the limbs (TAK is sometimes called the “pulseless disease”), low or high blood pressure, different blood pressure between arms and legs or sounds called “bruits” heard over the large arteries with a stethoscope.
- Blood tests: Two common blood tests that can help detect inflammation include the erythrocyte sedimentation rate (ESR) test, commonly called the “sed rate” and the C-reactive liver protein test (CRP). These tests, however, are not conclusive on their own and may be normal in up to 50 percent of patients with TAK.
- Imaging: Non-invasive tests such as magnetic resonance angiogram (MRA) and computed tomography angiography (CTA) are usually enough to establish the diagnosis. An angiogram (an X-ray of a blood vessel that has been injected with a special contrast dye) is rarely needed. Imaging tests can show narrowing or blockage of the vessels or the formation of an aneurysm—an abnormal bulge in the blood vessel that can burst, with life-threatening consequences. Your doctor may order other imaging tests as indicated including the Doppler ultrasound and positron emission tomography (PET) scan.
The goals of treatment include controlling inflammation of the blood vessels and preventing further damage. For some patients, the disease may go into remission and medication can be tapered or stopped. But for others, the disease may need to be controlled with medicine on a long-term basis. In severe cases, surgery may be required to bypass blocked vessels.
Initial treatment typically consists of glucocorticoids such as prednisone, starting at a high dose and then tapered down to minimize side effects. Other medications that suppress the immune system may be prescribed to achieve remission and reduce the need for prednisone. They include methotrexate, azathioprine, and mycophenolate mofetil.
Biologics: Those with severe disease who don’t respond to traditional treatments may be prescribed a biologic medication. Biologic drugs are complex proteins derived from living organisms. They target certain parts of the immune system to control inflammation. Among these, tocilizumab and infliximab have been used in TAK. Small studies show good results in controlling inflammation and reducing the need for glucocorticoids in TAK, but more research is needed.
Surgery: In cases where arteries have become severely narrowed or blocked or to repair aneurysms, vascular surgery may be required to improve blood flow.
Learn More About Treatments for Vasculitis
The medications used to treat TAK have potentially serious side effects such as lowering your body’s ability to fight infection, and potential bone loss (osteoporosis), among others. Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
Even with effective treatment, relapses can occur in individuals with TAK. If initial symptoms return or new ones develop, report them to your doctor as soon as possible. Regular checkups and ongoing monitoring of laboratory and imaging tests are important in detecting relapses early.
Effective treatment of TAK may require the coordinated efforts and ongoing care of a team of medical providers and specialists. In addition to a primary care provider, you may need to see a:
- Rheumatologist (joints, muscles, immune system)
- Cardiologist (heart)
- Vascular surgeon or other specialists
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of your health care team. It may be helpful to keep a health care journal to track medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, speak up. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
Learn More About Building Your Treatment Team
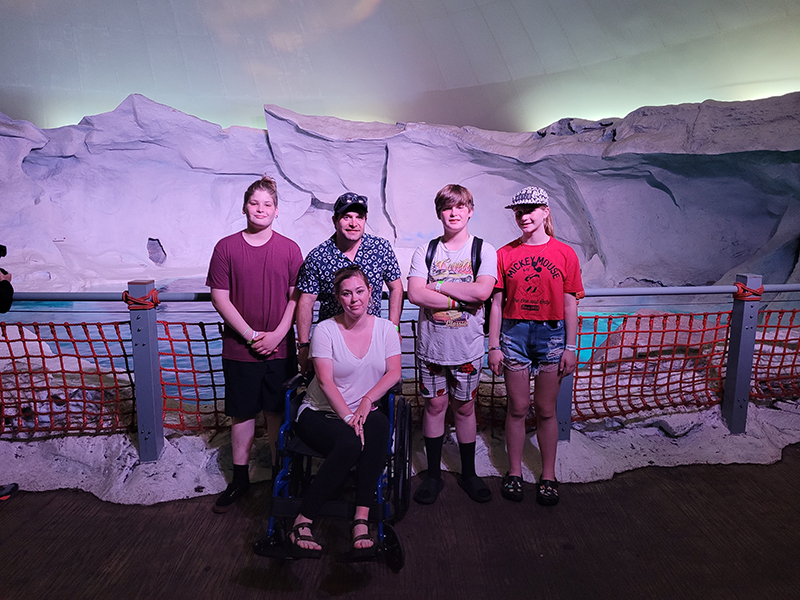
Living with Takayasu Arteritis
Coping with TAK can be overwhelming at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
There is no cure for TAK at this time, but with early detection, proper treatment and ongoing monitoring, many patients have a good prognosis. Imaging tests such as MRA and CTA scans remain the diagnostic tools of choice for this chronic disease, and are also used to monitor the blood vessels during and after treatment.
In 2021 the American College of Rheumatology (ACR) published guidelines for the management of certain vasculitides, that were also endorsed by the Vasculitis Foundation (VF). Clinical practice guidelines are developed to reduce inappropriate care, minimize geographic variations in practice patterns, and enable effective use of health care resources. Guidelines and recommendations developed and/or endorsed by the ACR are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The application of these guidelines should be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are subject to periodic revision as warranted by the evolution of medical knowledge, technology, and practice.
Takayasu Arteritis Videos
[youtube-feed feed=24]
